Mastering Wound Management: Your Guide to Swift Healing and Care
Wound management is a critical aspect of healthcare that involves assessing, treating, and caring for various types of wounds to promote healing, prevent infection, and minimize complications. Healthcare professionals encounter a wide range of wounds, including acute injuries, chronic ulcers, and surgical incisions, each requiring specialized care approaches.
Why is wound management important?
Proper wound care is essential because:
- It accelerates healing: Unmanaged wounds can take significantly longer, leading to complications.
- Reduces infection risk: Open wounds are susceptible to bacterial infections, which can cause severe complications such as sepsis.
- Prevents chronic wounds: Poor wound care can result in long-term wounds that fail to heal fully.
- Improves quality of life: Effective wound management reduces pain, improves mobility, and enhances overall patient well-being.
- Reduces healthcare costs: If not adequately treated, chronic wounds cost the U.S. healthcare system $28-31 billion annually.
 Types of Wounds and Their Challenges
Types of Wounds and Their Challenges
- Healthcare professionals encounter a variety of wounds, including:
- Surgical wounds: Post-surgery incisions that require specific care to prevent infections.
- Acute wounds: Caused by trauma (cuts, burns, surgical incisions) and typically heal within a few weeks.
- Chronic wounds: These include pressure ulcers, diabetic ulcers, and venous ulcers that persist for months due to underlying conditions. For example, a diabetic patient with a foot ulcer may struggle with healing due to poor circulation. Without proper wound management, the wound may worsen, potentially leading to amputation.
Understanding Wound Care Techniques

Wound Cleansing and Irrigation
Cleansing a wound is the first step in preventing infection and promoting healing.
Methods:
- Standard saline solution is commonly used as it is gentle and does not damage tissues.
- Antiseptic solutions may be used for infected wounds but should be cautiously applied to avoid tissue damage.
- Irrigation with a syringe can help remove debris and bacteria.
Example: A deep laceration from a fall should be thoroughly irrigated with saline to remove dirt and bacteria before dressing.
Stages in Wound Healing
The four stages of wound healing indicate inflammation stage 2, which is prevented with proper wound management and ends in a healed wound.
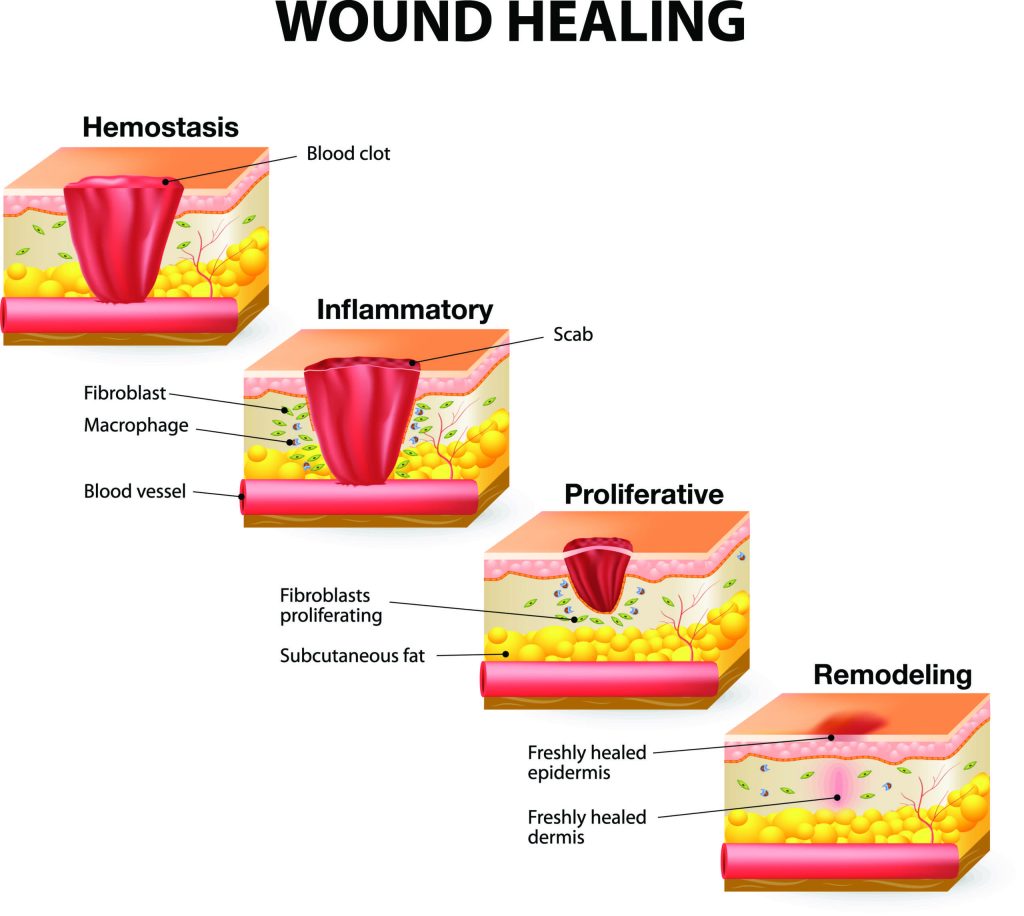
Source: https://www.shieldhealthcare.com/community/wound/2015/12/18/how-wounds-heal-the-4-main-phases-of-wound-healing/
Timeline of Wound Healing
- Minor Cuts & Scrapes → Heals in 3-7 days
- Surgical Wounds → Heals in 1-3 weeks
- Traumatic Wounds → Heals in 2-4 weeks
- Burns (1st & 2nd Degree) → Heals in 2-3+ weeks
- Chronic Wounds (Ulcers, Sores) → May take months or never fully heal
Choosing the Right Dressing

The choice of dressing depends on the type and severity of the wound.
Types of Wound Dressings
- Absorbent dressings (e.g., alginates, foams): These are used for heavily draining wounds. Weeping wounds with excess drainage can be treated with absorbent dressings like alginates or foams to manage moisture. However, it’s essential to maintain a moist wound environment to facilitate healing.
- Hydrocolloid dressings maintain a moist healing environment, ideal for pressure ulcers. They can promote faster healing and reduce the frequency of dressing changes.
- Silicone-based dressings are non-adherent wound contact dressings made from polyester mesh coated with soft silicone. They are gently adhered to the skin surrounding the wound, minimizing pain and trauma when changed. The dressing allows the passing of exudate.
- Negative Pressure Wound Therapy (NPWT): Suction removes excess fluid, reduces swelling, and promotes blood flow. It helps the wound heal faster by removing fluid and bacteria with suction. It also protects the wound from harmful things in the air, creating a suitable environment for healing.
Example: A patient with a large, weeping wound from a second-degree burn might require foam dressings to absorb drainage while keeping the wound moist.
Maintaining a Sterile Environment
1. Wound infections can delay healing and lead to severe complications.
2. Key Practices for Sterility:
- Use sterile gloves and dressings.
- Clean the wound with antiseptic techniques before applying a new dressing.
- Dispose of contaminated materials properly.
Example: In a hospital setting, wound infections significantly cause delayed healing, making sterile technique essential during dressing changes.
The Importance of a Wound Care Specialist

Healthcare professionals, particularly wound experts, play a vital role in this field.
- Manage complex and chronic wounds: Their expertise is especially critical in managing complex or chronic wounds.
- Chronic wounds affect approximately 8.2 million people in the U.S. and require specialized care.
- Specialists ensure proper wound healing by assessing the patient’s condition, selecting the appropriate treatment, and monitoring progress.
- They use advanced technologies such as NPWT and bioengineered skin substitutes.
- They educate patients on wound care best practices to prevent future complications.
When facing a wound, seek the help of an experienced wound care specialist. Proper care that accelerates healing, reduces infections, and improves patient quality of life will result. Book a wound management consultation at Kuye Medical Group for expert comprehensive care.






